Recently, the Neurology Specialty Group of the Pediatric Department at the Second Hospital of Shandong University, in collaboration with the Departments of Neurology, Pediatric Surgery, and Pathology, successfully conducted a multidisciplinary consultation for a rare case of DMD in a child with negative MLPA gene testing. This comprehensive approach provided the child with a one-stop multidisciplinary treatment plan for the rare disease.
In August of this year, the Pediatric Department of the Second Hospital of Shandong University admitted a 9-year-old male patient who had been experiencing reduced activity endurance for a year and a half. The patient had previously undergone MLPA gene testing at a local hospital, which did not identify any pathogenic genes. After detailed history-taking and thorough examination, Associate Chief Physician Guo Qinghui of the Pediatric Department preliminarily diagnosed the case as "Hereditary Muscular Disease - Progressive Muscular Dystrophy." In order to further confirm the diagnosis, and with the active cooperation and informed consent of the parents, genetic third-generation sequencing was performed on the child, along with first-generation validation for the child's parents and siblings. This was complemented by electromyography and lower limb soft tissue muscle MRI. A multidisciplinary consultation was conducted in conjunction with the Departments of Neurology, Pediatric Surgery, and Pathology. A muscle biopsy was performed on the child and sent for muscle pathological testing, ultimately confirming the diagnosis of Progressive MuscularDystrophy.

Progressive Muscular Dystrophy (PMD) is a rare neuromuscular disorder, inherited as an X-linked recessive genetic disease. It encompasses Duchenne Muscular Dystrophy (DMD) and Becker Muscular Dystrophy (BMD). Over a period of two to three decades, patients may progress from severe skeletal muscle dysfunction to respiratory muscle involvement, eventually leading to respiratory failure and death. Its progressive, life-threatening, and hereditary nature is deeply affecting. Due to its initially subtle presentation, diagnosis and treatment can be delayed. The early signs mainly manifest as delayed motor development. Many parents may not pay sufficient attention. Gradually, symptoms like limping and waddling gait may appear, followed by difficulties in standing and climbing stairs. The diagnosis of this disease relies on a neurological examination, laboratory tests (including enzyme spectrum, liver function, lactic acid, etc.), electromyography, and muscle magnetic resonance imaging, among other assessments. For the majority of patients, choosing the appropriate genetic testing is necessary for a definitive diagnosis. However, an exclusive focus on genetic testing should be avoided. It is crucial to consider the aforementioned diagnostic methods, and if necessary, perform a muscle biopsy for confirmation.
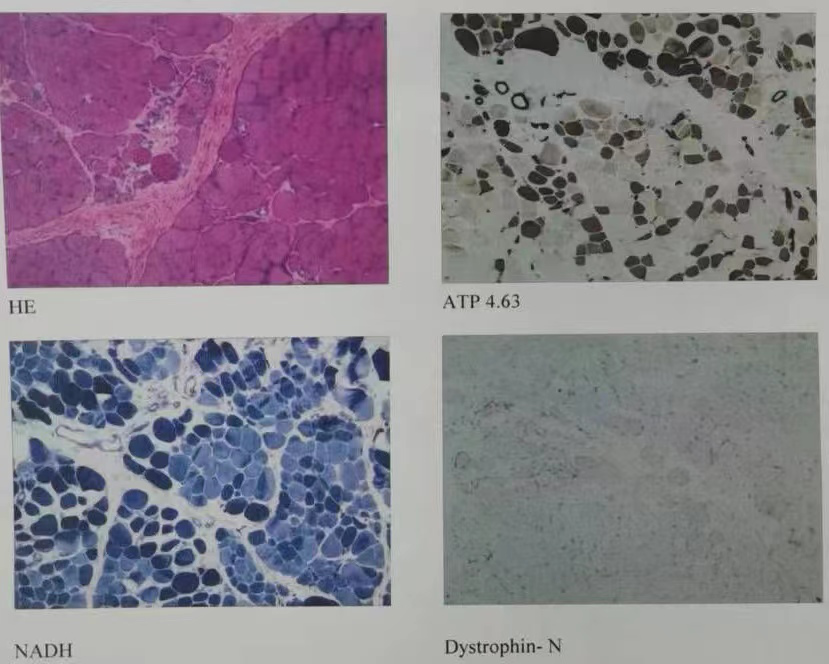
The child was immediately subjected to a multidisciplinary team (MDT) consultation upon admission. Under the guidance of Deputy Chief Physician JinSuqin from the Department of Neurology, muscle biopsies of the upper limbs were performed by Attending Physician Sun Xiaogang. Post-operatively, muscle pathology testing was conducted. Combining clinical presentations, electromyography, muscle soft tissue MRI, and the results of the muscle biopsy, a final diagnosis of Progressive Muscular Dystrophy was confirmed, and timely relevant treatment was administered.
In addition to the diagnosis and treatment of common pediatric neurological diseases and critical conditions, the Neurology Specialty Group of the Department of Pediatrics at the Second Hospital of Shandong University also addresses the diagnosis and treatment of rare pediatric neuro-muscular diseases, such as DMD, Myasthenia Gravis, movement disorders, Mitochondrial Encephalomyopathy, Lactic Acidosis, and Stroke-like Episodes (MELAS), among others.